Palliate
Supporting safer community palliative care with technology

Background
It is estimated that of the 6.2 million estimated carers in the UK, half a million are caring for someone with a terminal illness. The majority of those people who die every year would prefer to die at home, yet only about half achieve this.
This is often due to patients unable to have their symptoms managed properly at the end of life. People often have to wait longer than what feels acceptable to them for community nurses to come and administer medications or injections. When this happens, symptoms can escalate, carers and patients can become distressed and families lose control of the situation.
Such poor management of pain relief at the end of life can lead to unplanned emergency admissions, resulting in poorer quality of life and poorer experiences for carer and dying person.
Laycarers - family, friends or people important to the dying person - tend to the individual’s physical and emotional needs. They often wish they could do more, such as relieve community nursing teams of tasks like administration of medications. 39% of British adults say they would feel comfortable giving a pain-relief injection to someone who was dying and wanted to stay home, after receiving some training and with no additional support.
Training carers in the administration of end-of-life anticipatory (‘just in case’) medications for symptom control happens in the UK and abroad. Randomised control trials have shown that laycarers can confidently prepare and administer subcutaneous (under the skin) injections for palliative care patients in the home. The practice has been developed into various policies in England, Scotland and Australia, but it is not widespread.
Current and future provision of consistent, continuous care in the community rests on laycarers being properly trained to do more. There is huge potential to ‘upskill’ lay carers in the practical competencies required to care and support their loved ones in the community. We believe there should be a choice for carers to be trained to give symptom control medications. It’s important to note, though, that this is not an expectation, and carers must be deemed suitable by healthcare professionals.
We see the administration of medications by carers in the home, as a key element of good community care.
Introducing Palliate
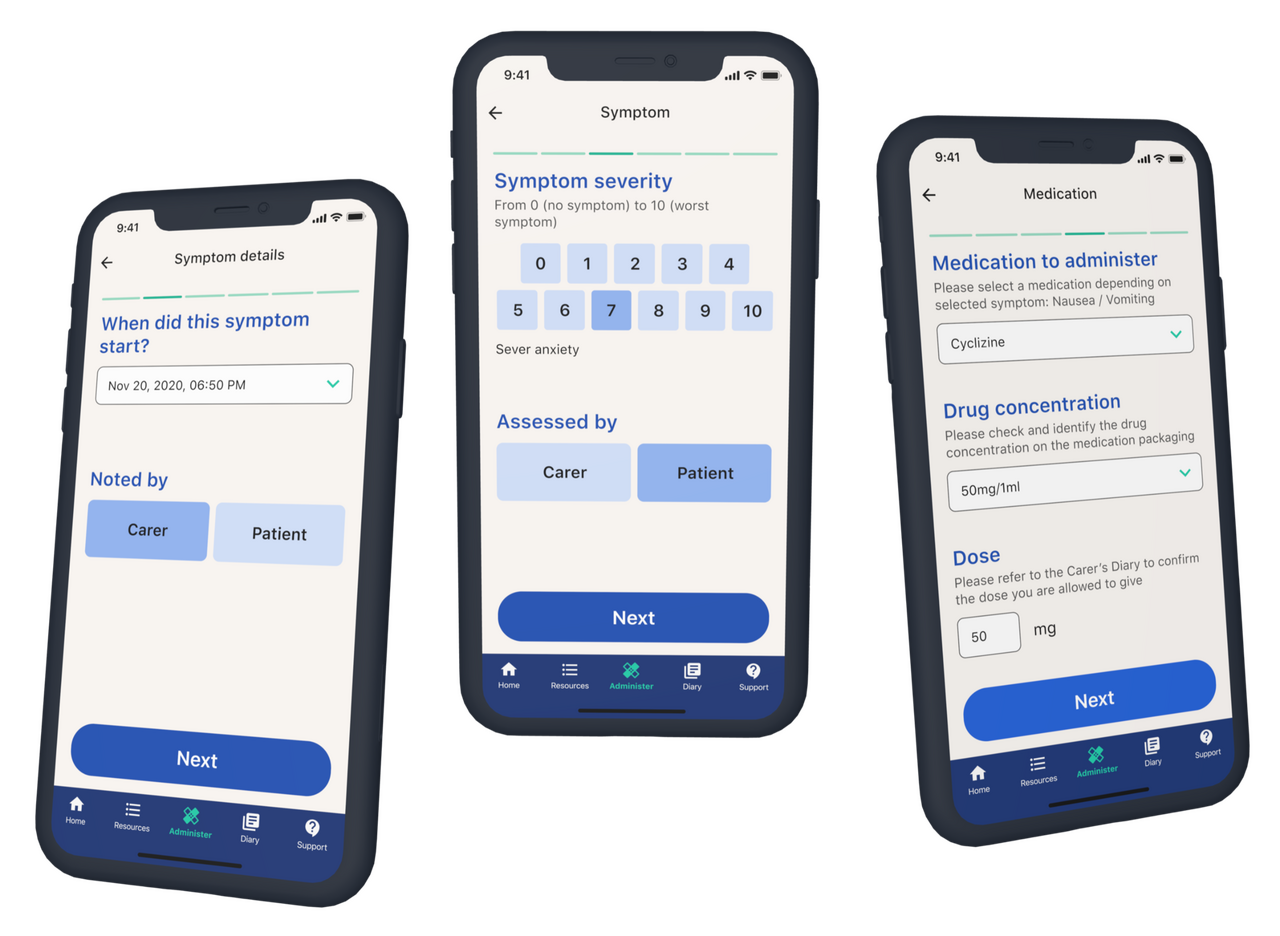
Palliate, is a healthcare intervention that seeks to improve the access and quality of training and support for carers to administer sub-cut medications in the home. In doing so, our ambition is to support patient preferences for a home death while also reducing pressure on community care teams. Palliate does this by providing digital information and support via an app, to carers who have been trained to deliver medications.
How we did it
In March 2020, we accelerated the early development of the project in response to COVID-19. The virus re-wrote the way in which end-of-life care was done in the community: district nurses and nurse specialists could no longer access patient homes, resulting in more families needing to do more themselves, in an uncertain environment. During the pandemic’s first wave, we rapidly deployed a website tool that incorporated Palliate’s training materials and processes, which was used by NHS and hospices teams across the UK.
From then, we have continued to work with NHS and hospice partners to develop a technology-driven support tool for carers. We aim to reduce friction in the experience of administering medications, improve the confidence levels of carers, improve the overall experience of managing symptoms and treatment in the home, and unlock opportunities for robust data collection for quality improvement and improved patient safety. In 2022, we undertook a small pre-pilot based in North Camden in London with CNWL NHS Trust, to test the intervention with volunteer families. They were given both a digital and paper-based version of the intervention, and followed the nurse-led training programme to safely and confidently administer medications.
Impact
As a result of our pre-pilot, we found that Palliate:
- was used confidently by carers (with an average confidence score of 8.73/10)
- 91% of injections were administered without healthcare professional assistance, highlighting the strength of the training material and ease-of-use.
- Importantly, the time between symptom onset and medication administration was reduced to from over 100 minutes to 20 minutes, meaning patients got the symptom relief they needed in a much reduced time. This resulted in improved carer confidence and better symptom management.
One carer reported: “I was able to improve symptoms, pain, distress, nausea….the ability to give an injection made a massive difference, most importantly for (patient) as the level of trust between us meant she wanted me to give it to her rather than other people, ie, HCP’s and this meant she was calmer as she trusted me. The short answer is that the alternative would have been calling for help and delays… the stress of someone unfamiliar always giving it to her would have made things much worse. There was no way to stop the whole thing (patient dying at home) from being stressful, but it was helpful to be in control. In some ways I felt calmer knowing and being in charge”.
Whats next
The work continues. In 2024, a mixed methods study - qualitative and quantitative studies - is to be conducted that explores the acceptability of the intervention for carers and capturing the perspectives of a wider range of professionals and public to understand the value of the intervention. This also includes further iteration and development of the Palliate product, with an expansion of the products with a healthcare professional view, to monitor patients remotely. Further piloting of the intervention in clinical environment with associated clinical studies, is planned for 2025.