Amber Care Plans
Digital services that facilitate difficult conversations
Background
Given the track record in changing how end-of-life care would be delivered, re-designing care planning became a major focus for us at the Helix Centre in 2017. We were excited by research showing advance care plans are effective in giving patients control during serious illness and death, and that people with a plan are more likely to die in their preferred place of care. We also believed that by combining our design and technical skills with insights from patients and their families, we could do something about the low take up of advance care plans.
As the population ages, and medical knowledge advances, the importance of giving people more choice and control over their care has never been greater. Around 500,000 people die each year in the UK, and half of these deaths occur in hospital. Yet only 8% of people want to be there.
Research shows that an advance care plan is an effective way to give people choice and control - 80% of people with a plan die in their preferred place of care. Having an advance care plan is highly effective in aligning healthcare with patients’ wishes. They reduce hospital bed days in over-65s and save money for the NHS. When an advance care plan is in place, patients and their families report happier experiences, particularly at the end of life.
An advance care plan is simply a guide spelling out your likes, dislikes, wishes, and the treatments someone would want to refuse or the rituals they would want followed - whether during illness or at the end of life. The planning process helps patients and those important to them think about different scenarios, and the plans are used by medical staff if the patient becomes too ill to communicate.
However, despite the numerous benefits only 5% of people admitted to hospital have an advance care plan. It’s like a will - we all should have one, but few of us bother until it is too late.
Our work
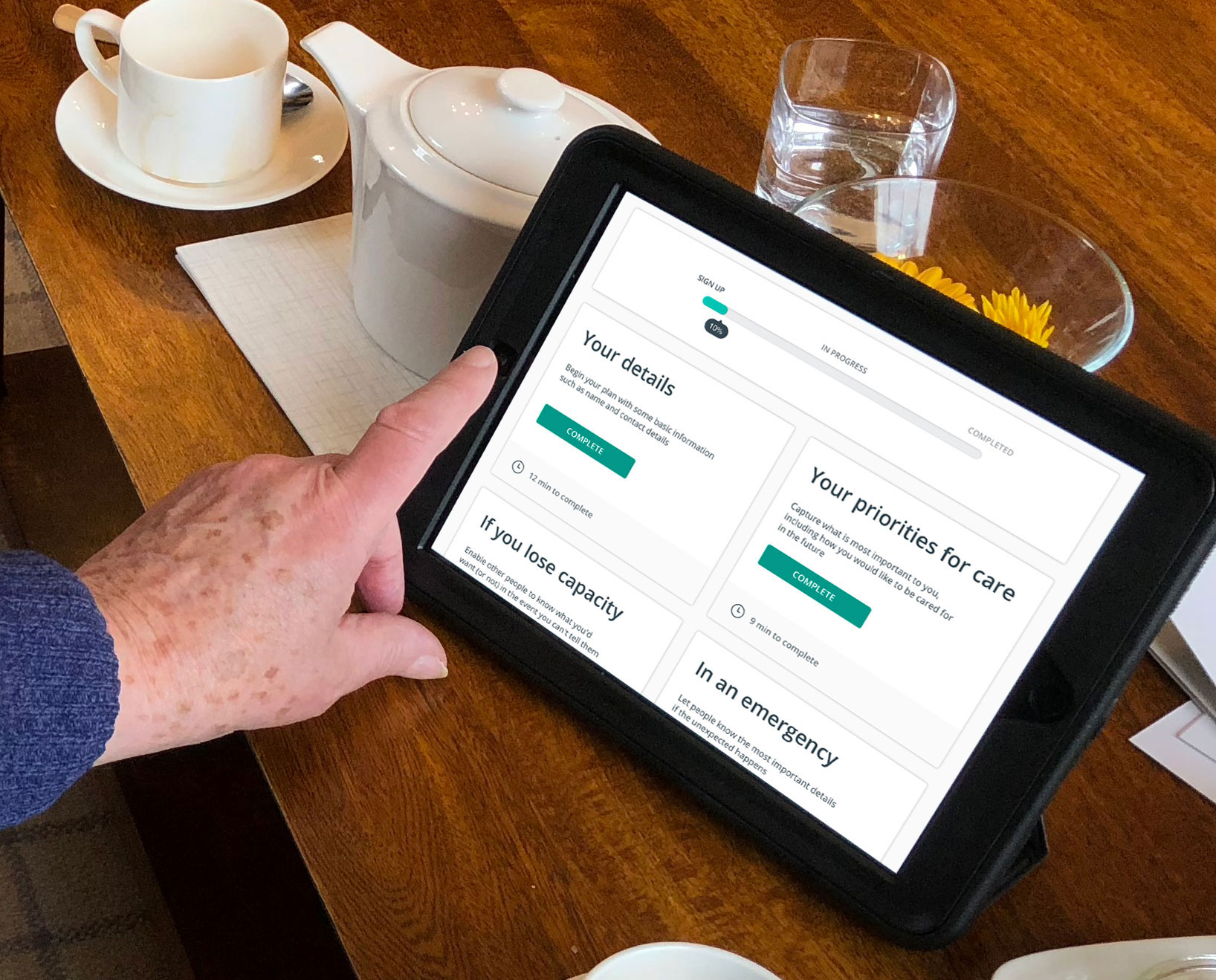
We wanted to change this, and from the outset we knew we didn’t just want to increase the number of plans being made in GP surgeries and hospitals. Clinicians are already very short on time. We wanted to take advance care planning mainstream – out of the clinics and hospitals, and into the home. We developed a digital platform designed to help individuals and families take an active role in planning and managing the care they receive, ultimately creating a plan that could be shared with family, carers and GPs.
To do this, we spun out a company, Digital Care Planning, with £500,000 funding from SBRI Healthcare, and brought the first product to market. The product, Amber Care Plans was designed to make the advance care planning process as easy as possible, so anyone can do it from the comfort of their own home.
During its development, our designs and prototypes were tested by volunteers from Marie Curie, and had invaluable input from Parkinson’s support groups and dementia memory clinics. We visited retirement communities and talked to GPs and palliative care consultants and tested the product with the public, at all ages.
We also developed an early AI-enabled chat bot that helped people think about and plan for end of life, and built a prototype voice bot, exploring the new technology at the time. It helped people consider different scenarios, and then they were offered a tailored template they could further personalise.
Impact
Sadly, despite the pre-seed funding, we were unable to develop a business model that would lead to sustainability whilst also meeting the complex needs of the NHS. Amber Care Plans was sadly shut down in the autumn of 2019 after running for 2 years, but its impact was felt widely. 4600 users signed up to make care plans with us, signing up 500 users a month at the time of closure. 40% of our users were living with an illness. Most were healthy, but just wanted to be well-prepared. Our completed digital plans equated to £3m in savings, with paper plans and partially completed plans giving a total of £9m in potential savings.